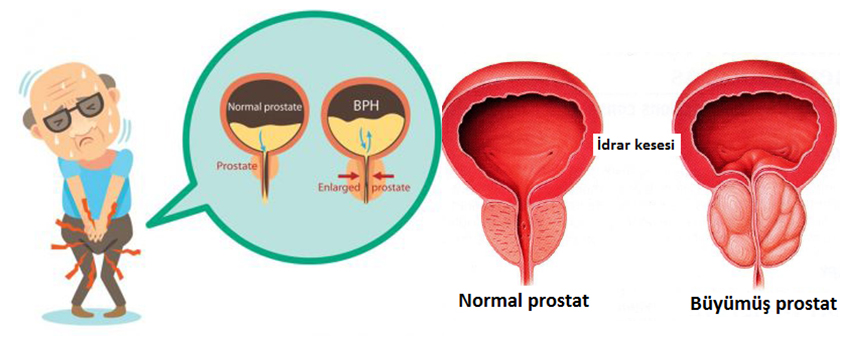
Prostate is a gland located in the lower urinary tract, in the lower part of the bladder (urinary bladder), around the urethra (the bladder outlet channel). Only in men. It secretes a liquid in the semen that feeds the sperm.
A healthy prostate is approximately the size of a large walnut and has a volume of 10-15 ml. As men get older, the prostate grows slowly.
Benign prostate enlargement
Prostate diseases usually occur later in life. Complaints may begin at the age of fifty and cause disturbing symptoms in the lower urinary tract in men. These symptoms are more often caused by the growth of the prostate, a disease known as benign prostatic enlargement. Some similar diseases can cause these complaints and your doctor will consider them.
Benign prostatic enlargement (BPH) affects your normal urination and reduces your quality of life, leading to lower urinary tract symptoms.
Prostate diseases can be very worrying, but it is important to know that BPH is not prostate cancer. However, benign prostate enlargement and prostate cancer may develop with age and may occur together. You should consult your urologist to address your concerns.
Symptoms of BPH:
Benign prostatic enlargement (BPH) can affect the urinary tract. This occurs because the enlarged prostate pressures the urinary tract at the bladder outlet.
Symptoms can sometimes be mild. For example, you may need to urinate more often or it may be difficult to empty your bladder fully. Your urologist may not offer treatment for these ambiguous symptoms and will follow up.
Symptoms can sometimes be very uncomfortable and may adversely affect your quality of life. In this case, you may benefit from the treatment.
These symptoms, often referred to as lower urinary tract symptoms, can often be caused by BPH and may be caused by other conditions affecting the excretory system.
Symptoms associated with benign prostate enlargement can affect urination in different ways:
*Effect on storage of urine in the bladder
*Effect on urination
*Effects after urination
*Symptoms of storage:
-The need to urinate more frequently than usual (frequency)
-Waking up to urinate at night (nocturia)
-The need for sudden urination and urgency
-Involuntary incontinence
*Symptoms of urination:
-Weak urination (dysuria)
-Bifurcated and dispersed urine flow
-Intermittent urination
-Urinate
-Waiting before urinating)
-It takes too long to urinate
*Symptoms after micturition:
-The feeling that the bladder is not fully emptied
-Involuntary incontinence in underwear after urination
Effects on your social life
Symptoms of BPH, such as a sudden feeling of urgency and the need to urinate frequently, can adversely affect your social life. Many patients are very uncomfortable with these symptoms and move away from social activities. They're afraid to be in a place where there's no toilet nearby. Long travel times come to the fearful dream judge. Because they often wake up at night to urinate and can't sleep enough, their energy levels fall and they have difficulty doing their daily activities.
BPH and sexuality
Symptoms of BPH can adversely affect your personal relationships and sexual life. Even if there is no direct organic connection, incontinence and sudden jams can disturb you. With impotence that develops with age, symptoms are confused and an inextricable appearance may occur. It may also be uncomfortable to talk about your sexual life, even if it is a urologist, but it is the most effective way to deal with your fears. Together with your partner or partner and urologist, you can set priorities in your sexual life and choose the most appropriate treatment. There are many ways you can relieve symptoms and improve your sex life, making it easier for you to live with BPH.
DIAGNOSIS
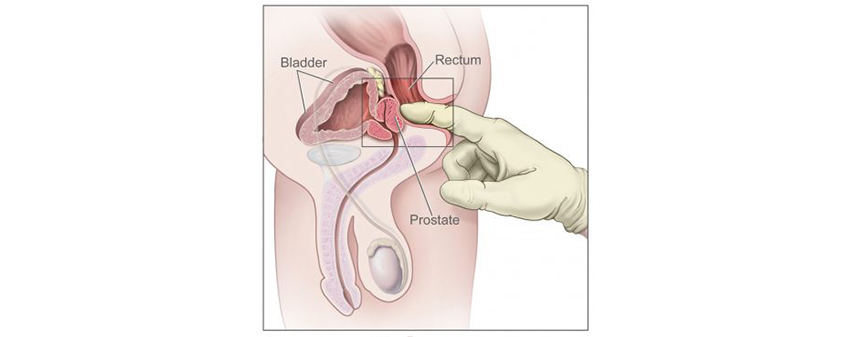
Your doctor will learn your medical history and perform a physical examination, including the necessary tests. During the examination, a finger can be used to understand the size, shape and stiffness of the prostate. Your symptoms will be carefully evaluated, blood and urine tests will be performed and your urine flow rate (uroflowmetry), will be measured. After voiding Urinary tract ultrasonography (USG) is extremely useful to measure the amount of residual urine remaining and to size the prostate.
Importance of PSA testing
Since benign prostate enlargement and prostate cancer can occur in the same age group, your blood PSA (prostate-specific antigen) test can be performed. PSA can also be used to predict your prostate volume and the risk of your benign prostate enlargement symptoms progressing. Among the causes of PSA elevation, BPH, prostate and urinary tract infections, prostate cancer, may occur in cases such as heavy exercise and your urologist will be able to classify these conditions in the most accurate way.
Urine analysis is performed to distinguish urinary tract infection that causes similar symptoms. If you have infection, urine culture is performed to confirm this and to choose the best antibiotic.
Uroflowmetry measures your urine flow rate. This test is used to determine if the prostate is blocking the flow of urine.
Measurement of urine (PMR) remaining in the bladder after voiding is done to determine if the bladder is fully emptied. Increased PMR is an indication that the bladder does not function well or that the voiding channel, called the urethra, is obstructed. This increases the risk of urinary tract infection.
Drug Treatment for Benign Prostate Growth
Drug treatment is recommended for patients diagnosed with benign prostate enlargement. This treatment is recommended when symptoms are uncomfortable and affect quality of life.
In the treatment of symptoms associated with BPH are used several groups of drugs:
Herbal Remedies
Alpha-blockers
5 Alpha-reductase inhibitors (5ARI)
Phosphodiesterase 5 inhibitors (PDE5)
Combinations of these drugs
Each group of drugs acts in a different way and have different effects and side effects.
What is wait-and-see treatment?
If you have mild lower urinary tract symptoms, you usually do not need medication or surgical intervention. In this case, your urologist will closely monitor your disease in the coming months or years and will start a different treatment when necessary. Your urologist will tell you about your disease, explain how you can develop, how to regulate your lifestyle, how to reduce your symptoms and how to deal with them.
Style changes in your life can help improve your BPH symptoms. For example, taking less fluid in the evening helps reduce urination at night. Consuming less alcohol, coffee or tea prevents bladder irritation.
Some men sit down and urinate to help empty the bladder completely. If you still feel it is not fully emptied, try again after 5-10 minutes.
Encourage yourself to hold your urine if you feel sudden congestion to urinate. This will accustom your bladder to keep more urine, so you will need to urinate less frequently.
Surgical treatment protocols in BPH.
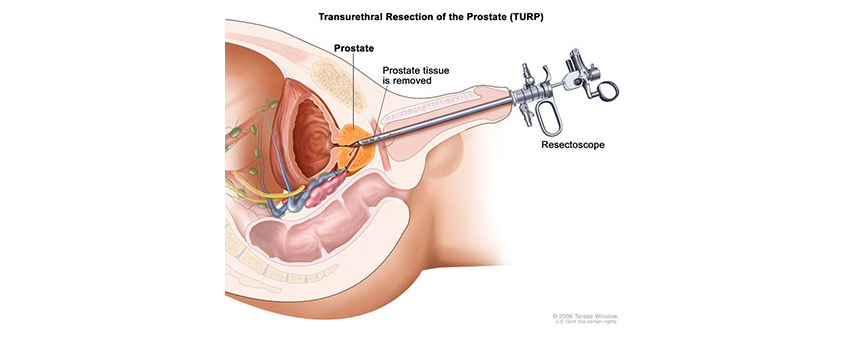
The most commonly recommended surgical treatment for BPH symptoms is transurethral resection of the prostate (TURP). The aim is to remove the prostate tissue (adenoma) that causes the symptoms with minimally invasive method. TURP provides optimal improvement of BPH symptoms.
Plasmakinetic: TUR is a modernized and advanced version and is one of the most widely used and reliable techniques. Less bleeding during the procedure, pathological material removal, easy and effective, shortage of complications and long-term results are among the advantages.
Transurethral prostate incision (TUIP): With this surgery, your doctor makes an incision from the bladder neck to the prostate to correct the urine flow. This procedure is rarely used in the treatment of BPH because it provides similar results to drug therapy.
Open prostatectomy: It is similar to TURP, but is made by incision in the abdomen. It is a rare procedure with the advancement of technology in older patients and may cause problems due to patient recovery time and complications.
Laser treatment: A laser using intense light is used to cut or vaporize the prostate. Very little blood is lost during the procedure.
Prostate stents: Stents are used to keep the urethra open and increase urine flow. It is recommended for men who are not suitable for surgery.
Transurethral needle ablation (TUNA): It is a minimally invasive treatment that uses heat (radiofrequency energy) to stiffen prostate tissue. The aim is to reduce prostate volume and improve symptoms.
Transurethral microwave therapy (TUMT) It is a minimally invasive treatment that uses microwave energy to stiffen prostate tissue. The aim is to reduce prostate volume and improve symptoms.
What is retrograde ejaculation?
During orgasm, the semen is no longer thrown out of the urethra, but is sprayed into the bladder and excreted in the urine from there. Retrograde ejaculation may develop after surgery for BPH. It is also linked to a number of types of drug treatment.
Is there a relationship between surgical treatment and erectile dysfunction?
Especially in closed surgeries where high technology is activated, sexual dysfunction after surgery is almost negligible.
Rarely, canal stenosis may develop after prostate surgery, mostly related to tissue type.